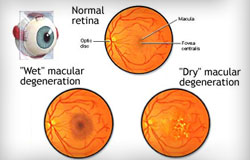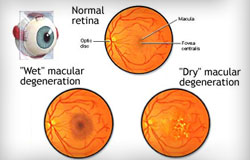
Age-related macular degeneration (AMD) is an eye disorder which usually affects older adults and results in a loss of vision in the center of the visual field (the macula) because of damage to the retina. It occurs in “wet” and “dry” forms. It is a major cause of blindness and visual impairment in adults older than 50 years old. People with macular degeneration often find it hard to recognize faces, read, and it can significantly affect their quality of life.
In the dry form of AMD, cellular debris accumulates in the macula (central part of the retina) and this is called drusen. In the wet form of AMD, new blood vessels grow in the layers of the macula and they bleed easily. However, macular degeneration will not lead to total blindness. In almost all cases, some vision remains. Approximately 10% of patients 66 to 74 years of age will have findings of macular degeneration. The prevalence increases to 30% in patients 75 to 85 years of age.
Risks for macular degeneration include high blood pressure, smoking, high cholesterol, obesity, consumption of large amounts of polyunsaturated fats, and Caucasian race. The lifetime risk of developing late-stage AMD is 50% for people who have a relative with AMD, versus 12% for people who do not have relatives with AMD.
Macular Degeneration Treatment for the dry form of AMD involves ultraviolet light protection, smoking cessation, diet modification, and an increased intake of two carotenoids, lutein and zeaxanthin. A good AMD Prevention Diet includes dark green vegetables, brightly colored fruits and vegetables, no simple sugars, cold water fish such as salmon, mackerel and sardines, and well as berries. Using olive oil or nut oil, as opposed to partially hydrogenated vegetable oil, is also beneficial. Consuming omega-3-fatty acids has been correlated with a reduced progression of AMD, also in conjunction with a low glycemic index diet. The Age-Related Eye Disease Study in 2001 showed that consumption of vitamins with high levels of vitamin C, vitamin E, beta-carotene, zinc and copper could help to delay the progression of dry AMD.
Treatment of the wet form of AMD uses injectable drugs that cause regression of the abnormal blood vessels in the macula. These drugs, called antiangiogenics or anti-vascular endothelial growth factors, are injected into the vitreous, which is the jelly-like portion in the back of the eye.
 512.263.1113
512.263.1113